LOADING
Heel pain can significantly affect mobility and daily activities. One common cause of this discomfort is plantar fasciitis, a condition that often results from repetitive stress on the foot. This article explores various treatment options, including the role of supportive insoles and stretches, to help manage pain and promote recovery.
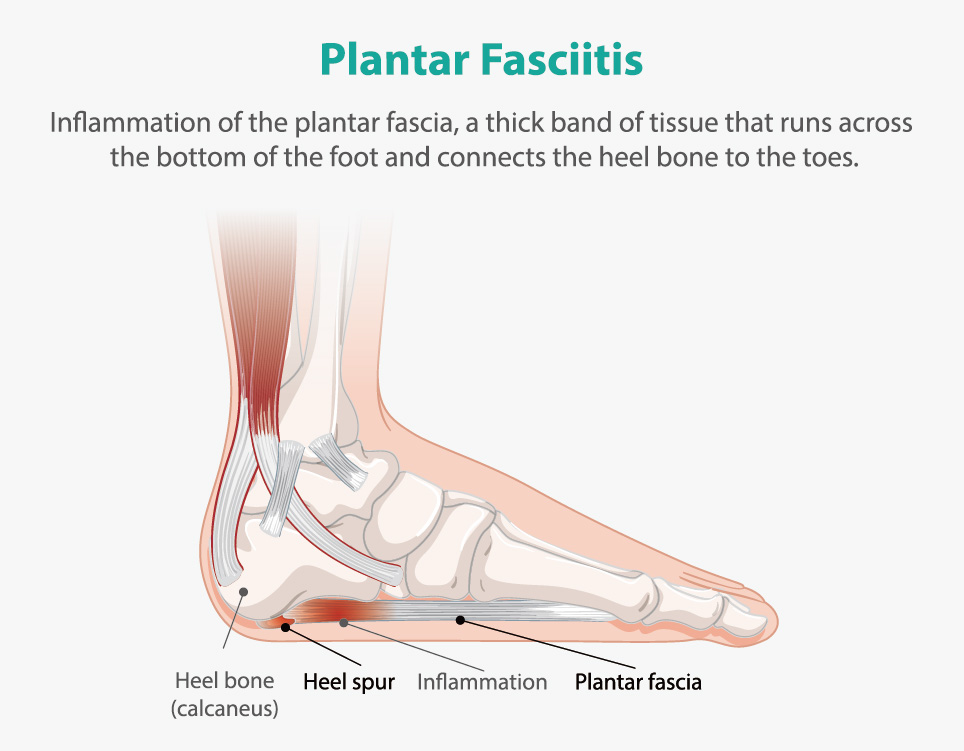
Plantar fasciitis is a common foot condition characterized by inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of your foot, connecting your heel bone to your toes. This inflammation typically causes heel pain, especially with the first steps in the morning or after periods of rest. It's a condition often associated with activities that put stress on the feet, such as running, walking, or standing for long periods, as well as factors like improper footwear, high arches, flat feet, obesity, and tight calf muscles. Proper diagnosis and management are essential to alleviate symptoms and prevent further complications.
Symptoms of plantar fasciitis typically manifest in the foot and heel area and may include:
The management of plantar fasciitis typically involves a combination of conservative treatments aimed at reducing inflammation, relieving pain, and promoting healing. Here are some common management strategies:

OPPO insoles and inserts can be beneficial in managing plantar fasciitis by providing support, cushioning, and proper alignment to the foot. Here's how they help:
OPPO inserts are designed to provide additional support to the arch of the foot, which can help distribute pressure more evenly along the plantar fascia. This reduces strain on the plantar fascia and alleviates pain associated with plantar fasciitis.
OPPO insoles and inserts are made with materials that offer cushioning and shock absorption, which can help reduce the impact on the heel and arch during activities like walking or running. This cushioning helps to lessen the stress on the plantar fascia and reduces pain.
OPPO inserts can help correct improper foot alignment, such as overpronation (rolling inward) or supination (rolling outward). By promoting proper foot alignment, orthotics help to prevent excessive strain on the plantar fascia and reduce the risk of injury or exacerbating plantar fasciitis symptoms.
Some OPPO inserts are designed to offload pressure from specific areas of the foot, such as the heel or the ball of the foot. By redistributing pressure away from sensitive areas, these inserts can help relieve pain and discomfort associated with plantar fasciitis.
Exercise plays a crucial role in the management of plantar fasciitis by stretching and strengthening the muscles and tissues in the foot and calf, improving flexibility, and reducing pain. Here are some effective exercises for plantar fasciitis:

Plantar Fascia Stretch: Sit on a chair and cross one foot over the opposite knee. Using one hand, pull back on the toes of the crossed foot, stretching the arch and bottom of the foot. Hold for 20-30 seconds, then release and switch feet.
Calf Stretch: Stand facing a wall with your hands resting on the wall at shoulder height. Place one foot forward and one foot back, keeping both heels flat on the ground. Gently lean forward, bending the front knee while keeping the back leg straight until you feel a stretch in the calf of the back leg. Hold for 20-30 seconds, then switch legs and repeat.
Toe Stretch: Sit on the floor with your legs extended in front of you. Use your hands to gently pull your toes back towards your shin until you feel a stretch along the bottom of your foot. Hold for 20-30 seconds, then release.
Calf Raises: Stand with your feet hip-width apart and hold onto a stable surface for support if needed. Slowly raise up onto your toes, lifting your heels off the ground as high as you can. Hold for a moment, then lower back down. Repeat for 10-15 repetitions.
Intrinsic Foot Muscle Strengthening: Sit in a chair with your feet flat on the floor. Spread your toes apart as wide as you can, then squeeze them together. Hold for 5-10 seconds, then release. Repeat for 10-15 repetitions.
Copy Link